Clinical History:
A 55-year-old female patient presented with complaints of abdominal pain in the right hypochondrium for 1 year. On USG two complex multiloculated cystic lesions were noted, one in each segment VII and VIII of the liver. CECT abdomen was advised for further evaluation.
Imaging Findings:
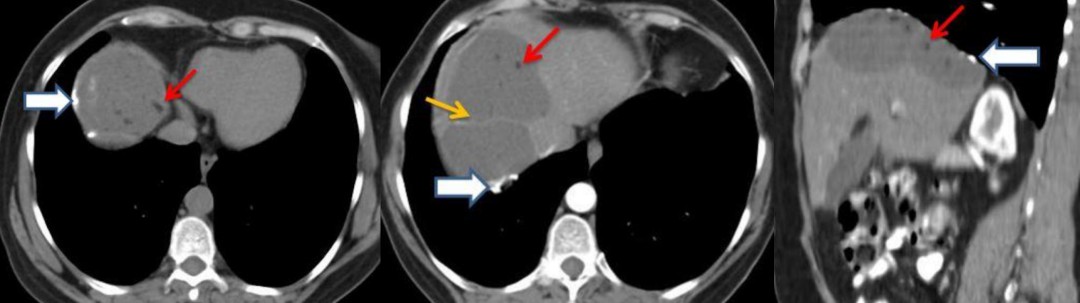
A rounded cystic lesion measuring approximately 74 mm (transverse) x 63 mm (AP) was noted in segment VIII of the right lobe of the liver. The lesion showed fluid density internal contents with fat density globules (red arrow) within. The cyst wall showed focal areas of dense calcification (white arrow). Another similar cystic lesion measuring approximately 62 x 62 mm was seen in segment VII of the liver. Thin septa (yellow arrow) was seen separating the two cysts. On a post-contrast scan the cyst wall showed mild enhancement. No evidence of a fat-fluid level. No evidence of any daughter cysts within. No features suggestive of cyst rupture or infection. No evidence of intrahepatic biliary radical dilatation or demonstrable cysto-biliary communication. The rest of the liver parenchyma appeared normal (Fig. 1 , 2 , 3). The findings were suggestive of hydatid cyst with possible degeneration.

Figure-1
Description: Axial non-contrast CT image shows well-defined cyst in segment VIII of the liver with wall
calcification (white arrow) and intracystic fat globules (red arrow).
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune
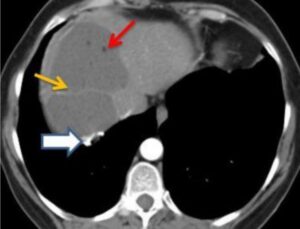
Figure-2
Description: Axial CECT examination image shows a thin enhancing septa (yellow arrow) separating
the two cysts with cyst wall calcification (white arrow) and intracystic fat globules (red arrow).
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune

Figure-3
Description: Sagittal reformatted CT image showing cysts in segments VII and VIII of the liver with cyst
wall calcification (white arrow) and intracystic fat globules (red arrow)
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune
Discussion:
Hydatid cyst is a disease caused by the larva of tapeworm, Echinococcus granulosus [1]. Depending on the stage of the cyst, growth imaging findings of Hepatic Hydatid Cyst (HHC) include unilocular cyst, daughter vesicles with daughter cysts, partially calcified or completely calcified/dead cyst [2]. Calcification can occur in the cyst wall or internally in the matrix.
Complications of HHC include infection and rupture. CT is imaging modality of choice for diagnosing cyst infection which appears as poorly defined masses showing rim enhancement representing abscesses with adjacent patchy enhancing liver parenchyma due to inflammation. Gas or air-fluid levels can also be seen within the cyst. HHC rupture occurs in 20% to 50% of patients [3, 4]. Assumed causes of rupture include degeneration of membranes, simple ageing of the cyst, trauma or chemical reactions [1]. There are three different types of cyst rupture: contained, direct and communicating.
In contained rupture endocyst ruptures, pericyst is intact with floating membranes within. Communicating rupture implies passage of the cyst contents into the biliary radicles. In direct rupture both endocyst and pericyst ruptures allowing free spillage of material into the peritoneal, pleural cavity, abdominal wall and hollow viscera. Fat-fluid level within the cyst has been described as an indirect sign of biliary communication [5]. Various studies show that there are two possible causes for the presence of fat within a HHC. A study series of three patients with HHC, concluded that the presence of lipid/fat globules within the hydatid cyst is to be due to a cysto-biliary communication [6].
Another study suggested that lipids play an important role in the metabolism of HHCs and that fat-fluid level in a HHC is related to degeneration of hydatid membranes (ageing process of the cyst) [7].
Surgery is the treatment of choice in cases of complicated cysts (rupture, cysto-biliary fistulas and secondary bacterial infection) [7]. In uncomplicated cysts, percutaneous USG guided drainage techniques like PAIR (puncture-aspiration-injection-reaspiration) and other modified catheterisation techniques with injection of scolicidal agents have shown excellent results [8].
Our case was managed with surgical excision of the cysts. CT is the modality of choice in identifying complications of HHC. Fat density in HHC is a rare finding. If fat fluid level is noted in the HHC, it favours the presence of a biliary communication which can be demonstrated on imaging.
However, if the small lipid / fat globules are noted within the cyst along with the presence of cyst wall calcification, as ain our case, it is more in favour of cyst degeneration than bilio-cystic communication.
Differential Diagnosis List:
Degenerating hepatic hydatid cyst showing fat globules and wall calcification., Hepatic angiomyolipoma, Hepatic teratoma
Final Diagnosis:
Degenerating hepatic hydatid cyst showing fat globules and wall calcification.
References:
Beggs I (1985) The radiology of hydatid disease. AJR Am J Roentgenol 145:639–48 (PMID: 3895873)
Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS (2000) Hydatid disease: radiologic and pathologic features and complications. Radiographics 20:795-817 (PMID: 10835129)
de Diego Choliz J, Lecumberri Olaverri FJ, Franquet Casas T, Ostiz Zubieta S (1982) Computed tomography in hepatic echinococcosis. AJR Am J Roentgenol 139:699-702 (PMID: 6981931)
Marti-Bonmati L, Menor Serrano F (1990) Complications of hepatic hydatid cysts: ultrasound, computed tomography, and magnetic resonance diagnosis. Gastrointest Radiol 15:119-25 (PMID: 2180773)
Mendez Montero JV, Arrazola Garcia J, Lopez Lafuente J, Antela Lopez J, Mendez Fernandez R, Saiz Ayala A (1996) Fat-fluid level in hepatic hydatic cyst: a new sign of rupture into the biliary tree?. Am J Roentgenol 167:91-4 (PMID: 8659428)
Beric V, Blomley M (1997) Re: Fat-fluid level in hepatic hydatid cyst: a new sign of rupture into the biliary tree?. AJR Am J Roentgenol 168:1381-2 (PMID: 9129453)
Malik Ajaz A., Bari Shams UL., Amin Ruquia, Jan Masooda (2010) Surgical management of complicated hydatid cysts of the liver. World J Gastrointest Surg 27;2(3):78–84 (PMID: 21160854)
Zargar SA (2011) Percutaneous drainage of liver hydatid cysts: is evidence enough to accept it as first modality of choice?. Trop Gastroenterol 32(3):161-3. (PMID: 22332329)