Clinical History:
A 22-year-old male patient with dwarfism presented with abdominal pain, bilateral lower limb swelling and fatigue with features of hypothyroidism. The patient’s blood counts were within normal limits.
Imaging Findings:
Axial pre (Fig. 1) and post-contrast (Fig. 2) CT of the abdomen was performed with coronal (Fig. 3, 4) reconstructions. It showed large well-defined lesions involving both kidneys with large fatty component and few large nodular soft tissue lesions within. The nodular component showed moderate homogeneous enhancement on contrast study. A large non-enhancing fatty component was noted. The lesion was predominantly involving medulla of the kidneys with distortion of a pelvicalyceal system. Thinning of renal parenchyma was noted with mild hydronephrosis in bilateral kidneys. The lesions were measuring 16x14x11cm (CCxAPxTrans) on the right side and 12x8x7cm (CCxAPxTrans) on the left side. There were no calcifications and no vascular elements in the lesions. Bilateral renal veins, arteries and IVC were normal. No e/o lymphadenopathy. No ascites. No focal hepatic lesion.
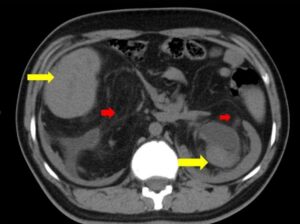
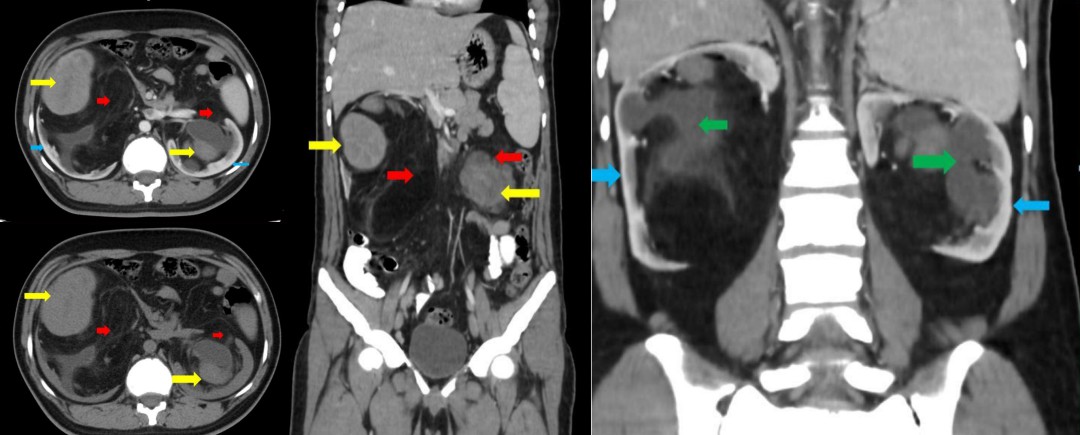
Figure-1
Description: Axial plain CT abdomen showing large well-defined lesions involving medulla of both
kidneys with large fatty component (red arrow) and few nodular soft tissue lesions (yellow arrow)
causing thinning of renal cortices (blue arrow)
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune
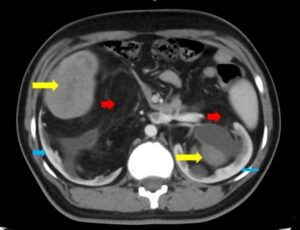
Figure-2
Description: Axial contrast CT abdomen showing moderate homogeneous enhancement of large
nodular soft tissue component (yellow arrow). No enhancement noted in large fatty component (red
arrow). Thinning of renal cortices (blue arrow).
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune

Figure-3
Description: Coronal contrast CT abdomen showing myelolipoma with predominant involvement of
renal medulla and moderately enhancing nodular soft tissue component (yellow arrow) and
nonenhancing fatty component (red arrow).
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune

Figure-4
Description: Coronal postcontrast CT image showing bilateral mild hydronephrosis (green arrow).
Thinning of renal cortices (blue arrow)
Origin: © Krsnaa Diagnostics Pvt Ltd, Chinchwad, Pune
Discussion:
Myelolipomas are benign mesenchymal tumours composed of adipose tissue and haematopoietic elements. The most common location for myelolipomas are the adrenal glands. They are rarely reported in extra-adrenal sites such as presacral region, pelvis, mediastinum, retroperitoneum and very rarely the renal parenchyma. Occurrence in extra-adrenal sites is 0.4% [1]. Extra-adrenal myelolipomas occur more commonly in women than in men and in older patients [2]. Pathogenesis of this tumour is not yet clear. Most of the theories postulate proliferation of ectopic adrenal or haematopoietic cell rests in response to stimuli like endocrine dysfunction [3]. Certain chromosomal translocations may be associated indicating it to be of bone marrow origin [4]. These tumours are frequently asymptomatic and occur in the setting of endocrine dysfunction. Patients might present with pain in abdomen due to intratumoural haemorrhage or infarction or mechanical compression of other structures by the tumour. Renal myelolipomas have an appearance of well-defined heterogeneous predominantly fat-containing lesions on CT. Fat displays low attenuation on CT (i.e.–25 to-100 HU). Enhancing soft tissue nodules represent myeloid component. Calcification can be seen rarely. On MRI, fat within the lesion displays hyperintense signal on T1WI with suppression on fat-saturated sequences. Myeloid components have a high signal on T2WI. Myeloid components show contrast enhancement. For the definitive diagnosis, FNAC or biopsy should be considered. A risk of intralesional haemorrhage should be considered. On histology, adipose tissue mixed with haematopoietic tissue (with granulocytic, erythropoietic and megakaryocytic lineages) is seen in variable percentage with no evidence of malignancy. Based on imaging, differential diagnosis of fat containing renal lesions should be considered including angiomyolipomas, liposarcoma and renal extramedullary haematopoiesis. Angiomyolipomas (AML) are benign mesenchymal tumours. They are cortically based usually small lesions. When large they have an exophytic component with wedge-shaped cortical defect indicating renal cortical origin. Intralesional vascularity and aneurysms are seen. Histologically AMLs have dysmorphic blood vessels, smooth muscle cells and adipose tissue which differentiates them from myelolipomas. Renal extramedullary haematopoiesis is a rare lesion, occurring in a different clinical setting of bone marrow disorders [2]. Patients are usually symptomatic with altered blood counts. They have predominant haematopoietic component and a lesser percentage of adipose tissue as opposed to myelolipoma. Renal liposarcomas are relatively rare; histologically they have lipoblasts and do not contain haematopoietic tissue. Prognosis of renal myelolipomas is excellent. Radiological follow up is needed in larger lesions as in our case for risk of haemorrhage. Symptomatic lesions may need surgical intervention.
Differential Diagnosis List:
Renal myelolipoma, Extramedullary haematopoiesis, Renal angiomyolipoma
Final Diagnosis:
Renal myelolipoma
References:
Prahlow JA, Loggie BW, Cappellari JO, Scharhng JO, Teot A, Iskandar SS (1995) Extra-adrenal myelolipoma: report of two cases. South Med J 88(6):639–643 (PMID: 7777880)
George SA, Manipadam MT, Thomas R (2012) Primary myelolipoma presenting as a nasal cavity polyp: a case report and review of the literature. J Med Case Reports 6:127 (PMID: 22584001)
Hunter SB, Schemankewitz EH, Patterson C, Varma VA (1992) Extra-adrenal myelolipoma: a report of two cases. Am J Clin Pathol 97:402–404 (PMID: 154316)
Bishop E, Eble JN, Cheng L, Wang M, Chase DR, Orazi A, O’Malley DP (2006) Adrenal myelolipomas show non[1]random X-chromosome inactivation in hematopoietic elements and fat: support for a clonal origin of myelolipomas. Am J Surg Pathol 30(7):838–843 (PMID: 16819325)